









The binocular slit-lamp examination provides a stereoscopic magnified view of the eye structures in detail, enabling anatomical diagnoses to be made for a variety of eye conditions. A second, hand-held lens is used to examine the retina. A slit-lamp exam is usually done during a regular checkup with your eye doctor before the cataract surgery procedure.
NC Tonometer is used to perform Tonometry. Tonometry is a quick and simple test that checks the pressure inside your eyes. The results can help your doctor see if you're at risk for glaucoma. The pressure inside your eye is called intraocular pressure (IOP).
This test measures fluid pressure in your eye. The test involves using a slit lamp equipped with forehead and chin supports and a tiny, flat-tipped cone that gently comes into contact with your cornea. The test measures the amount of force needed to temporarily flatten a part of your cornea.
Gonioscopy is an eye test that checks for signs of glaucoma. It uses a special lens and slit lamp to evaluate your eye's drainage angle (anterior chamber angle). If the drainage angle is blocked or closed, you may have glaucoma. Gonioscopy is one of many tests you may need if you are at risk for glaucoma.
This lens provides ultra resolution with radinal image with the binocular indirect ophthalmoscope during clinical practice or in the operating room.
Ophthalmoscopy is a test that look at the back of the eye called the fundus. The fundus consists of the retina, optic disc and blood vessels.
A direct ophthalmoscope is a device that produces an unreversed or upright image of around 15 x magnification.
An indirect ophthalmoscope produces a reversed or inverted image with 2 to 5 x magnification.
A visual field test measures how far the eye sees in any direction without moving and how sensitive the vision is in different parts of the visual field. This helps doctors to find certain types of injuries and disease, like glaucoma
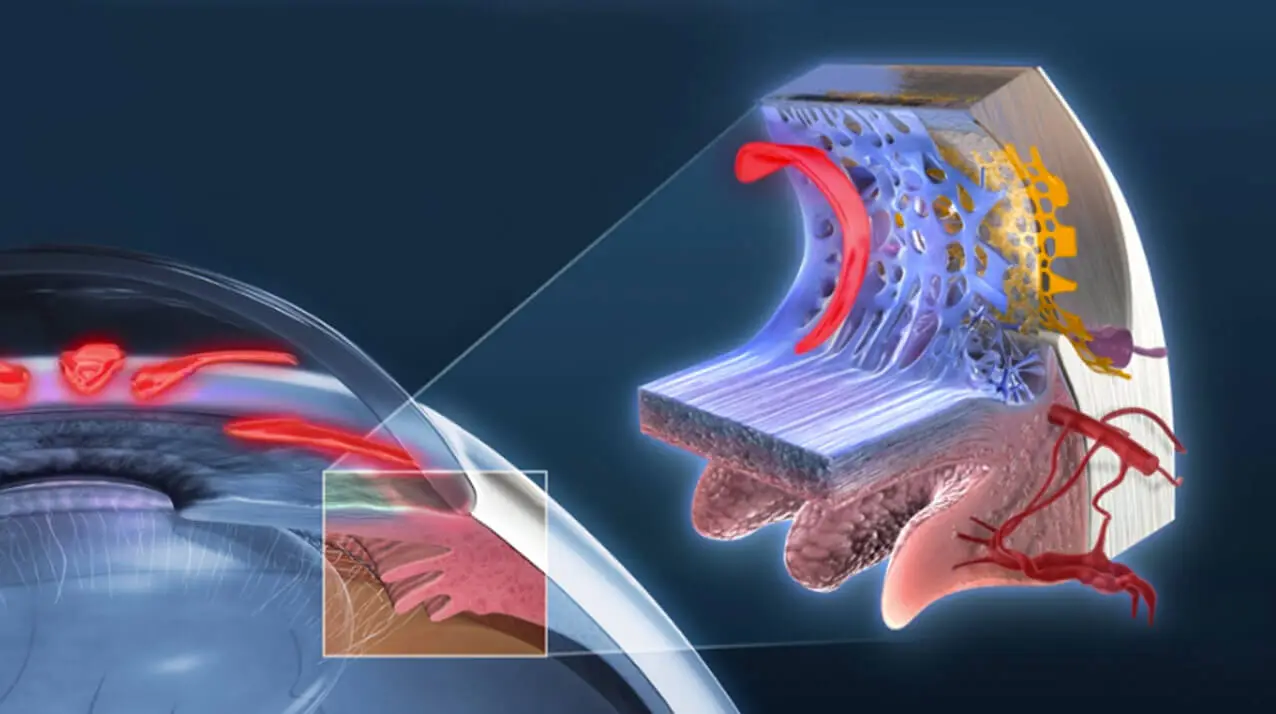
Optical Coherence Tomography (OCT) is an imaging method used to generate a picture of the back of the eye, called the retina. OCT uses light waves to take cross-section pictures of your retina. The OCT is an excellent way to visualize the different layers of the retina and optic nerve in the eye. OCT is routinely used during check-up of patients with glaucoma.
Color Fundus Retinal Photography uses a fundus camera to record color images of the condition of the interior surface of the eye, in order to document the presence of disorders and monitor their change over time.
A fundus camera or retinal camera is a specialized low power microscope with an attached camera designed to photograph the interior surface of the eye, including the retina, retinal vasculature, optic disc, macula, and posterior pole (i.e. the fundus).
An operating surgical microscope is the most important optical instrument in the modern era of ophthalmic surgeries. It provides the surgeon with a magnified and illuminated high-quality image of the small ophthalmic structures. Being binocular the surgical microscopes gives the additional benefit of high-quality stereoscopy. Our microscopes are high-end with video recording facilities.
A pachymeter is a medical device used by the doctor to do a test called pachymetry. It is a simple, quick, painless test to measure the thickness of your cornea. With this measurement, your doctor can better understand your IOP reading, and develop a treatment plan that is right for your condition. The procedure takes only about few minutes to measure both eyes.












There is no single value to be considered normal eye pressure. On average, your eye pressure should be within 10-22mmHg but it also depends on various other factors like gender, age, ethnicity, hereditary, and corneal thickness to name a few.
Every individual above the age of 40 years must have an annual ophthalmic evaluation, however glaucoma screening is must if there is a family history of glaucoma, systemic disease such as diabetes/hypertension, high myopia, history of trauma to the eye, long term steroid use.
The frequency of follow up is usually decided by your doctor, based on the severity of the disease. It is important to ensure regular follow ups to prevent worsening of the disease.
No,the existing nerve damage is not reversible. However, timely intervention and regular follow ups can prevent the progression of the disease.
Most people with glaucoma can still drive. Your ability to drive will depend on how much field of vision has been lost. Your doctor will perform regular visual field tests to evaluate the same.
You must continue routine timely instillation of medications until the earliest time you can visit your doctor.
To minimize systemic absorption, close your eyes for one/ two minutes after putting the eye drops. You may then press lightly at the corner of your eye near your nose to close the tear duct for one/ two minutes. Wipe off excess eye drops from your eyelid. If you have more than one eye drop, space them at 5 minutes interval between each drop.
It is usually rare. However,due to systemic absorption some individuals may experience dizziness, decreased heart rate, excacerbation of asthma, impotence, tingling sensation of extremities, fatigue, metallic taste, frequent urination, dry mouth etc. depending on the medication you are using. Always consult your doctor if you experience any new systemic effects after starting any medication.
Angle is the space between the clear part (cornea) of the eye and coloured part (iris) of the eye through which the aqueous flows out of the eye.
In closed angle glaucoma the angle becomes narrow or closed causing either sudden increase in eye pressure or a gradual increase which could lead to optic nerve damage and possible vision loss.
It is done as an OPD procedure.
Prior to treatment, eye drops are instilled in the eyes to make the pupil small. This may take about 1-2 hours.
Just before the procedure, anaesthetic drops are applied to numb the surface of the eye
A lens is then placed on the eye to perform the laser procedure.
It usually takes about 10-15minutes to complete the procedure in both eyes.
There could be temporary blurring of vision, redness of the eye or increases sensitivity to light. These usually subside within a day. Anti-inflammatory drops are prescribed after the procedure and the eye pressure is assessed after 1 week.
Not always. In case of an acute attack of angle closure, the patient experiences blurred vision due to collection of fluid in the clear part of the eye( cornea). The peripheral iridotomy helps relieve the blockage of fluid outflow and clears the cornea. This restores the vision to pre attack status. However the procedure is meant to preserve the existing vision and prevent glaucoma progression.
In majority of cases, the procedure carries little to no risks. The documented risks are closure of irodotomy requiring re-treatment, excessive bleeding (especially in patients on blood thinners), progression of cataract, rarely retinal and choroidal detachments. Your doctor will discuss your risk profile with you and take necessary precautions.
Although it is unusual, serious complications such as infection, bleeding in the eye, loss of vision and eye pressure that is too low or high can occur. Therefore, regular follow ups to monitor the eye pressure, surgical wound and bleb along with disease progression is important even after the surgery.
Most patients do not require medications to control the eye pressure post trabeculectomy. Some patients continue to progress despite surgical intervention. In such patients if your doctor feels the eye pressure is not optimal or if there is a progression you may be advised to continue using the eyedrops.
Usually it is a safe procedure to control the eye pressure, but certain complications like infection, tube extrusion, corneal decompensation, implant failure may occur. These complications can occur any number of years post surgery. Hence
regular follow up as advised by your doctor is important to optimize your results.
It is a relatively safe procedure, complications like inflammatory reaction, pain, red eye, conjunctival scarring, extremely low eye pressure and further vision loss may occur in rare cases.
1, Tapovan Society Nr. Nehrunagar Cross Road Satellite, Ahmedabad, Gujarat - 380015 | TEL: +91 7926753534
Opp. Z. K. Hotel Relief Road, Ahmedabad, Gujarat - 380001 | TEL: +91 7925506257
307-311, Iconic Isanpur, Near Honda showroom, Next to Indian Oil Petrol Pump, Naroda Narol Highway, Isanpur, Ahmedabad, Gujarat - 382443 | TEL: +91 9979393783
102,103, B Square 2, Vikram Nagar, Iscon-Ambli-Bopal Road, Ahmedabad, Gujarat - 380054 | TEL: +91 8160755086